Atrial fibrillation (AFib) is a condition that affects millions of individuals in the United States. It occurs when the heart’s rhythm becomes irregular, causing the upper chambers of the heart (atria) to beat out of sync with the lower chambers (ventricles). Understanding AFib and working with a cardiologist are key steps in managing this condition. Here is more information on what this condition is, its causes, symptoms, methods of diagnosis, and how it can be effectively managed:
What Is Atrial Fibrillation?
Atrial fibrillation, commonly referred to as AFib, is a type of irregular heart rhythm, or arrhythmia, that originates in the atria. The atria, or the upper chambers of the heart, beat erratically during an AFib episode, causing the heart to lose its usual rhythm. Instead of contracting rhythmically, the atria quiver or fibrillate, disrupting normal blood flow.
AFib can occur in brief episodes, or it may be persistent, requiring medical attention to restore a regular heart rhythm. While not immediately life-threatening, it is associated with an increased risk of complications. This includes stroke, heart failure, and other cardiovascular issues.
What Causes It?
There are many potential causes of this condition. It is often linked to underlying conditions that affect the heart’s structure or function. High blood pressure, heart disease, and abnormalities in the heart’s electrical pathways are common contributors.
Other triggers include thyroid disorders, excessive alcohol consumption, or chronic illnesses like diabetes. Certain temporary conditions, such as dehydration or infections, may also initiate AFib episodes. Some individuals may experience atrial fibrillation with no identifiable cause.
What Are the Symptoms?
Not all individuals with this condition experience symptoms, but those who do may notice various physical changes. Symptoms include:
- Irregular or rapid heartbeat
- Feeling of fluttering or palpitations in the chest
- Fatigue or reduced ability to exercise
- Dizziness or lightheadedness
- Shortness of breath
- Chest discomfort or pain
Some symptoms can occur intermittently, even resolving on their own, while others persist and require medical attention.
How Is Atrial Fibrillation Diagnosed?
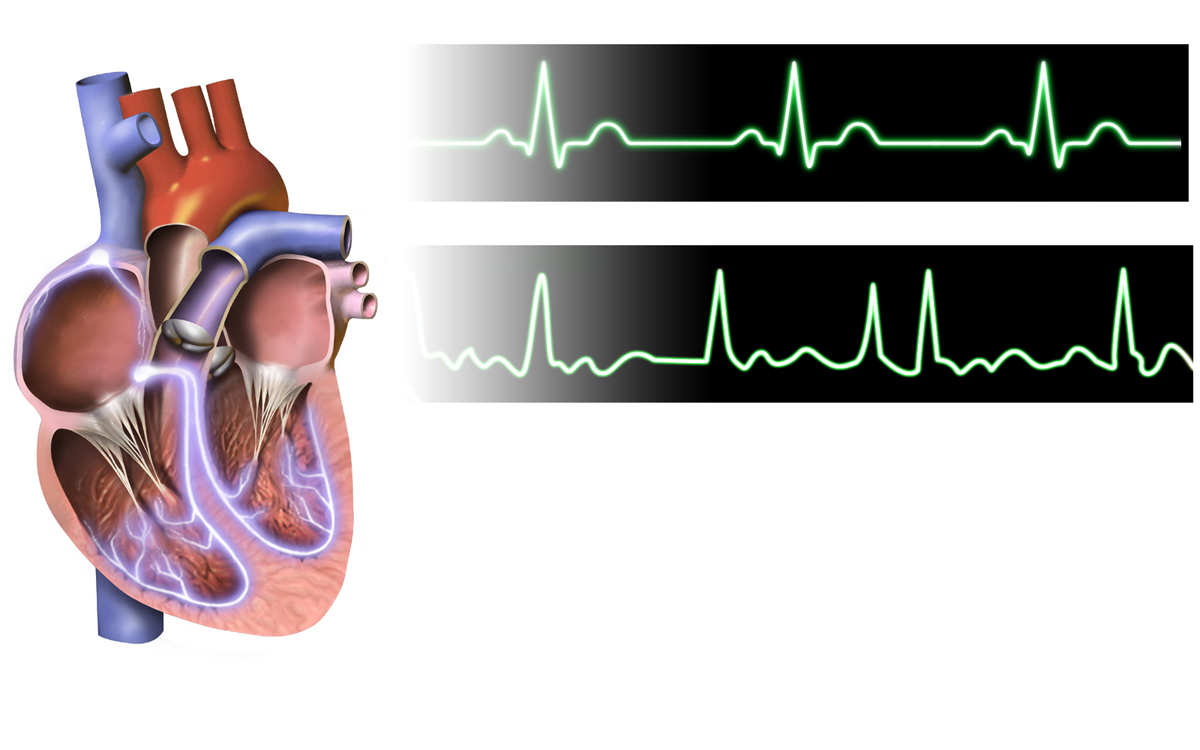
Diagnosing this condition typically involves reviewing the patient’s medical history and symptoms. A physical examination may reveal signs of AFib, such as an irregular pulse. Following the initial assessment, cardiologists use diagnostic tools like electrocardiograms (EKGs) to confirm the presence of atrial fibrillation.
An EKG records the heart’s electrical activity and can detect the erratic rhythm characteristic of AFib. If episodes are intermittent, a longer-term monitoring device such as a Holter monitor may be used to capture irregular rhythms over a period of days or weeks. Blood tests or imaging tests, including echocardiograms, may also be ordered to check for underlying conditions.
How Does a Cardiologist Help Manage It?
Cardiologists play a key role in diagnosing, treating, and helping manage atrial fibrillation. Treatment plans often vary based on the underlying cause, the patient’s symptoms, and the presence of risk factors for complications like stroke. Cardiologists aim to restore normal sinus rhythm, control heart rate, and reduce the risk of blood clots.
Medications are a common first step in managing AFib. Cardiologists may recommend procedures like electrical cardioversion, which uses controlled electric shocks to reset the heart rhythm, for symptom relief and long-term control. Lifestyle changes can also help improve outcomes. Cardiologists may advise patients to adopt a heart-healthy diet, increase physical activity, or reduce alcohol consumption.
See a Cardiologist Today
Atrial fibrillation is manageable with proper care and guidance from a cardiologist. Early diagnosis and treatment can reduce the risk of complications, helping patients maintain a healthy, active lifestyle. Schedule an appointment with a cardiologist to take the first step toward effective management.
- FREHF – The Revolutionary Future Of Human-Centered Technology!
- Adsy.Pw/Hb3 – Boost Your SEO And Drive More Traffic!
- Fitness Based Vacations By Timeshealthmage.com!
- TimesHealthMag Tips For Improving Sleep Quality – Expert Advice For Better Rest!
- How TimesHealthMage Helps Improve Your Lifestyle Habits!

Leave a Reply